Skin fungus is the most common dermatological disease. But the defeat on the legs is considered the most common. Mycoses of the legs and onychomycosis are often found in those who visit public places, in particular hospitals, saunas, baths, swimming pools and gyms.
Each type of fungus has its own characteristics, signs and methods of treatment that you need to know for those who are at risk of contracting a fungal infection.
What is foot mycosis?
Mycosis, or ringworm, is a dermatological disease caused by a fungal pathogen. The fungus of the skin of the legs is the most common type of this disease, since it is on the legs that the skin is more sensitive, which, moreover, is constantly exposed to the external environment affected by fungi.
Risk factors
Foot athlete's foot is common in men who prefer completely closed shoes. Feet begin to sweat and a breeding environment develops. Therefore, most men who have served in the army know firsthand what a skin fungus is. In children, fungal infections occur due to non-compliance with hygiene rules, walking barefoot on contaminated soil and non-compliance with sanitary standards in kindergartens.

Often, fungal infections of the feet are also found in women with hormonal disorders or a decrease in immunity during pregnancy. Infection can also occur during a pedicure through non-sterile instruments or towels.
There are common factors that provoke the development of the disease:
- Wearing too tight shoes made of synthetic materials.
- Infrequent washing of feet, wearing dirty socks.
- Wearing someone else's shoes, using someone else's towels and other hygiene items.
- Diseases that disrupt blood circulation in the lower extremities.
- Disorders of the immune system.
- Failure to comply with hygiene rules in public places.
- The presence of corns, wounds and cracks on the feet.
- Long-term treatment with antibiotics or corticosteroids.
Psychosomatics
The causes of the fungus can also be in the emotional state of a person. The medical direction that studies the psychological state of a person and its influence on the development of bodily diseases - psychosomatics - explains fungal infections by the suppression of negative emotions held back inside.
Constant feelings of resentment, anger, feelings of betrayal, or frustration can trigger the fungus or prevent a person from fully recovering.
As a result of these conditions, human immunity is reduced, pathogens present in the body are activated. People with a chronic fungal infection that does not go away with drug treatment need to reconsider their internal state or consult a psychologist.
According to many scientists who have studied the psychosomatic causes of the fungus, if you do not work on your character and get rid of negative emotions, then the disease will return again and again.
pathogens
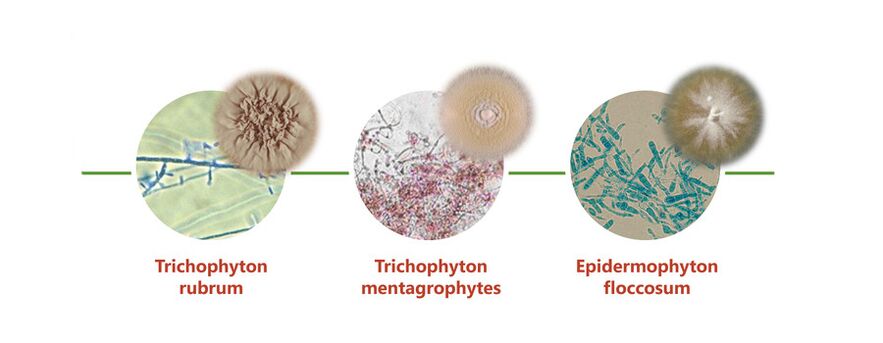
There are a large number of pathogenic microorganisms that can cause human skin lesions, but the following types of fungus are most often localized on the legs:
- Trichophyton rubrum, or Tripchophyton purpureum- cause rubromycosis, a disease that most often affects the skin of the feet and nails, but can also spread to other parts of the body.
- Trichophyton interdigitale, or Trichophyton mentagrophytes (Trichophytons)- cause epidermophytosis, which develops between the fingers, but can also go to the entire area of the foot.
- Candida- candida rarely occurs on the feet, but can also affect the interdigital space, nails and the sole of the foot. It develops predominantly in females.
Mycosis is an infection, and infection can occur in two ways: directly - directly from an infected person to a person, and indirectly - through the floor, shoes, clothes and other household items with which the infected person has come into contact. It is very easy to get infected with a fungus of the lower extremities - just a second contact with any surface or object touched by a person with a fungal infection is enough.
The mechanism of development of fungal diseases begins from the moment the spores enter the human skin. If the conditions are favorable, then development, growth and reproduction begin.
Microorganisms begin to secrete enzymes that destroy keratin proteins, and, accordingly, the stratum corneum of the skin. Hence, itching and discomfort arise in humans. The infection spreads very quickly, fungi penetrate into the deeper layers of the skin and infect the surrounding tissues.
If you do not start treatment, then very quickly large areas of the skin are affected.
But not always the infection develops immediately after infection, sometimes the fungi remain on the skin or shoes for a long period of time. But as soon as the body's defenses decrease, or a favorable warm and humid environment develops, fungi begin to develop rapidly.
General symptoms
Ringworm of the lower extremities is a very common infection that requires immediate treatment. But not everyone immediately turns to a specialist for help, as they do not pay attention to the primary symptoms or believe that these are signs of other dermatological diseases.
Common signs of infection of the skin are:
- Redness and peeling of individual areas.
- The appearance of blisters or cracks.
- Feeling of itching and burning.
- Dryness and roughness of the skin.
But depending on the localization and pathogen, the disease proceeds with various clinical manifestations. The fungus on the heels begins with reddening of the skin and a burning sensation. Over time, bubbles appear, which, bursting, form very painful sores.
Then cracks and growths with peeling form. With a long course of the disease, an unpleasant odor begins to emanate from the affected area, and the infection passes to other areas of the feet and nails.
Fungus on the knees is rare, but if cracks appear on or under the knee that do not go away for a long time, then you need to see a doctor. Usually, the fungus in this area begins imperceptibly - it starts with redness, then the peeling of the skin intensifies, very rarely bubbles form on the surface of the spot, which eventually become covered with scabs.
Damage to the nails - onychomycosis - begins with infection of the skin of the feet. In this case, itching and cracks may appear on the skin, but sometimes fungi do not touch the skin, affecting only the nail plate.
Stages:
- Normotrophic- at this stage, only the color of the nail begins to change - it becomes yellow, sometimes with a brown tint.
- Hypertrophic- the healthy shine of the nail disappears, it becomes irregular in shape, thickens and begins to partially collapse. A person may feel pain while wearing tight shoes.
- Onycholytic- the diseased nail is a plate with crumbling layers, becomes thinner, takes on a brown color. At this stage, detachment from the nail bed begins.
Manifestations of different types of pathology
Candidiasis of the legs affects only soft areas of the skin and nails, without affecting the feet, it can be of two types:
- vesicular-pustular- at the first stage, reddening of the skin with pronounced edema appears. In the future, the affected area is covered with bubbles filled with liquid or purulent mass, in the process they burst, forming erosion. Gradually, the inflammatory process decreases, and peeling increases on the foci.
- Hyperkeratotic- is rare, characterized by a thickening of the stratum corneum with the formation of scaly burgundy furrows.
In most cases, the fungus between the toes is epidermotrophy. Skin changes in this pathology may have.jpg) the following forms:
the following forms:
- squamous- between the third and fourth fingers, the skin begins to redden and sometimes itch. Very often this stage is overlooked.
- Intertriginous- develops from the first stage. Edema develops, cracks form, and the lesion spreads to neighboring areas. Growths form around the diseased area, making it difficult to wear shoes.
- Acute- large accumulations of bubbles filled with liquid are formed. Wounds and cracks begin to hurt, the general state of health worsens, the temperature may rise.
When the condition is neglected, interdigital pathology covers the nails and the entire area of the sole of the foot, that is, epidermotrophy of the feet develops. External symptoms are similar to weeping eczema, which complicates the diagnosis.
Rubromycosis of the feet is a simultaneous lesion of the interdigital folds. The skin becomes drier, reddens, severe peeling begins. If treatment is not started in a timely manner, then the process passes to the sole, the lateral area of the feet and the surface of the fingers.
Rubromycosis can also affect other areas of the legs: shins, thighs, buttocks, as well as any parts of the body and head. The lesions are pink patches covered with scaly skin, vesicles, or a crust. They quickly grow in size, merging with each other. Rubromycosis of smooth skin usually proceeds in an acute form and is accompanied by severe itching.
"I got cracks on my foot, but I didn’t pay attention. The fungus was discovered during a medical examination at work. The doctor immediately prescribed ointment and pills, she also scolded that she did not immediately apply. "
The specifics of traditional treatment
Therapy of the fungus on the legs is based on the application of antifungal external agents to the lesions. There are a lot of drugs in the form of ointments, creams, sprays, solutions. Their action is aimed at suppressing the vital activity and reproduction of fungi, as well as slowing down the process of their spread.
Recently, various sprays from the fungus have appeared, which are very convenient to use for external use in the treatment of skin and nail fungus.
During therapy, you can process shoes and clothes so as not to provoke re-infection. Disinfectant sprays are suitable for this. Treatment can also be carried out with antiseptics.
You can use antifungal agents in the form of solutions.
Before applying ointments, you can use a regular alcohol salicylic solution. It actively acts on fungi, simultaneously relieves inflammation and dries weeping skin areas.
In case of damage to the nails, it is recommended to use special antifungal varnishes.
There are a lot of different external remedies and all of them can be purchased at the pharmacy without a prescription. But for the treatment to be effective, you need to know how to use external agents correctly:
- Follow the instructions for the frequency of application of the drug.
- Hard areas must be steamed before applying the external agent.
- With large dry growths, you can make a bath with soda.
- Treat only affected areas, without affecting healthy skin.
- After treatment, wash your hands thoroughly, without touching other parts of the body, so as not to spread the infection.
In advanced cases, you need to take tablets from the fungus at the same time as using external agents.You can not take pills inside without the recommendation of a doctor - only a specialist can prescribe drugs, based on the type of pathogen and the severity of the course of the disease.
Treatment of a fungal lesion on the legs at an early stage will not take much time, provided that the drugs are used correctly and the instructions are followed. In severe cases, long-term treatment, up to 3-6 months, may be required. If the prescribed drugs do not give the desired effect, then you need to contact a specialist and get new recommendations.
"The fungus on the lower extremities was treated with different ointments for my husband, I tried 8 different pieces, but only tablets from the group of triazole derivatives helped. Well, externally he continued to smear allylamine cream.
Folk methods of treatment
Very often, non-traditional methods are used to treat fungus on the nails and legs.But patients should remember that such remedies are effective at the initial stage of the fungus, and in severe cases, they can not always help, but, on the contrary, aggravate the course of the disease.
Before you get rid of the fungus on the feet with folk remedies, you need to visit a doctor to establish an accurate diagnosis, since the symptoms can indicate various dermatological diseases.

Herbs from the fungus are used to prepare baths, rubbing and lotions:
- Pour a handful of calendula flowers with 50 ml of alcohol and 100 ml of water and leave for a day in a dark place. Use for rubbing twice a day. Best for nail infections and skin candidiasis.
- Mix dry mint leaves and fine salt in equal proportions. Apply to the affected areas for a day, securing with a bandage. After the time has elapsed, remove the bandage, wash your feet, dry and repeat. Use only on nails and keratinized skin.
- Five tablespoons of dry celandine pour 100 ml of vodka, leave for two weeks. Use for wiping, trying to avoid contact with healthy skin.
- Brew two tablespoons of thyme in a glass of boiling water, leave for an hour and use for lotions.
You can use tar soap from the fungus:
- Grate a bar of soap, add a little water and melt in a water bath, add a spoonful of tar and 2 tablespoons of any oil. Mix thoroughly and pour into molds to make a healing soap. Use to wash your feet.
- Mix a tablespoon of crushed soap with 2 teaspoons of soda and add a little water to make a thick mixture. Apply to clean feet at night, and apply a bandage on top.
- In the initial course of the disease, it is enough to apply soap suds from laundry soap to the affected areas of the skin and leave for 15-30 minutes.
Effective garlic for fungus:
- Apply crushed garlic to the steamed areas and secure with a bandage. Keep all night.
- Within 3 days, insist a mixture of garlic juice, water and vodka, taken in equal proportions. Rub 1-2 times a day on the affected areas.
- Pour 2 finely chopped cloves of garlic into a glass of vinegar. Infuse in a dark place for 2 weeks in a container with a closed lid. Use for rubbing and lotions.
Vinegar can be used for rubbing or bathing. To prepare a bath, you need to take 100 ml of 9% table or apple cider vinegar for 1 liter of water. The duration of the procedure is 15 minutes, after which you need to remove the softened skin and put on clean socks.
"At work, I walk in shoes for days, my feet constantly sweat, and a fungus often appears on the foot, I immediately start making baths with vinegar and process all my shoes with it. It goes by very quickly. "
Consequences and predictions
Many believe that the fungus is not harmful, except for aesthetic discomfort. But fungal infections also carry other threats. First of all, there is a danger of the fungus spreading to other areas of the skin.
From the feet, the infection passes to the skin of the hands, face, torso, scalp. This happens if you do not wash your hands after touching the affected areas of the skin or if the patient's immunity is greatly reduced. From an infected person, infection of family members occurs if sanitation rules are not followed.
With deep lesions, it becomes impossible to wear habitual shoes, there is severe pain when walking, and when the nails are damaged, the nail bed rises. There is a risk of inflammation of the nerve endings.
Skin lesions, if left untreated, provoke the addition of viral and bacterial infections. The following complications often occur:
- Warts.
- Phlegmon.
- Pyoderma.
- Erysipelas.
- Malignant mycosis fungoides.
A fungus of the skin on the legs with a long course worsens the functioning of the immune system, patients become more susceptible to allergic manifestations, urticaria, bronchial asthma, conjunctivitis and rhinitis. Often, mycoses are accompanied by atopic dermatitis and eczema. The general condition worsens, weakness occurs, body temperature may periodically rise.
Running yeast infections can provoke damage to internal organs.
In addition to physical complications, fungal infections lead to instability of the psycho-emotional state. Infected people become irritable, quick-tempered, and often lash out at others. The instability of the nervous system slows down recovery, so patients may need psychological support.
Toe fungus is very easy to cure if you start therapy at the very first manifestations of the disease. With daily use of therapeutic agents, the fungus can be eliminated in 10-14 days. But with an advanced infection, treatment will be longer and more difficult and will not do without the use of systemic drugs. Therefore, doctors recommend not to delay visiting the clinic.















